Summary:
Tuberculosis (TB) has been present since ancient times and still has significant burden worldwide. Even with availability of antibiotics and anti-tubercular drugs that have proven high efficacy the control of disease has been tough. In addition, Multidrug-resistance (MDR) and Extensively drug resistant (XDR) Tuberculosis has brought additional challenge for the health system. To end TB by 2030, we need innovative and effective intervention that are backed up by advancement in the field of prevention control and management.
Brief Background:
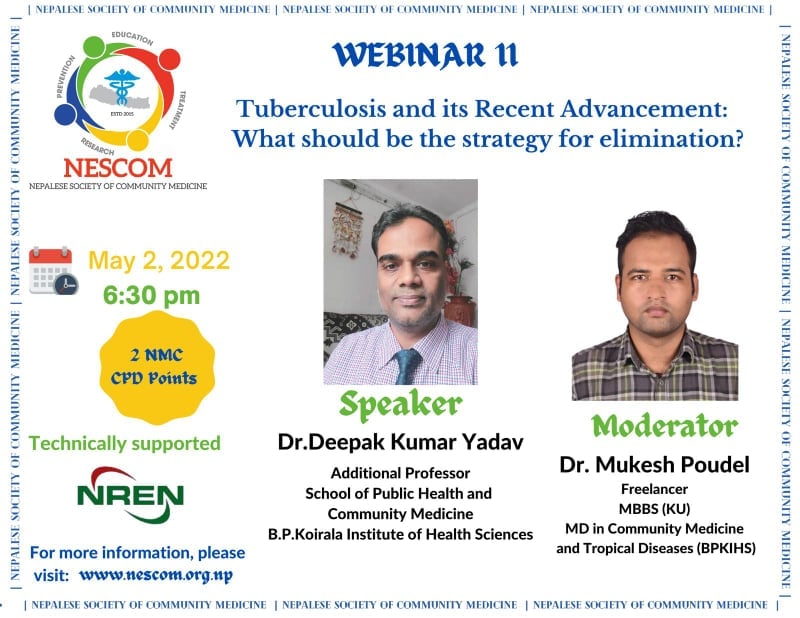
The proceedings of the webinar was started by Master of Ceremony, Dr. Rajiv Mani Adhikari where he introduced the speaker Dr. Deepak Kumar Yadav and the moderator Dr. Mukesh Poudel. Dr. Yadav works at School of Public health & Community Medicine, B.P. Koirala Institute of Health Sciences, Dharan as a faculty since 2008. He holds various positions in different National and International bodies in Nepal and has received awards for his contribution in field of Tuberculosis control. He is currently working in the Multinational Project: Antimicrobial Resistance and Labor Migration across Healthcare Boundaries. Dr. Poudel who was the moderator of the program currently works at the Consultant for development of National Aviation Public Health Emergency Preparedness Plan. He has previously worked as a Specialist Doctor in Ministry of Social Development, Bagmati Province and in Epidemiology and Disease Control division, Department of Health Services, Nepal.
The presentation started with the justification of topic,Tuberculosis and its recent advancement: What should be the strategy for elimination?, by Dr. Yadav where he focused on how TB has been present in the community as a fatal disease since ancient time and even with availability of effective treatment how it still is one of the leading cause of deaths worldwide. He emphasized on TB being a major cause of burden of the disease on every individual of the world whether rich or poor and especially affecting the marginalized poor population. He further gave an insight on the global burden of TB epidemic followed by its burden in Nepal. Global milestones that was achieved and that are planned to be achieved to End TB was also highlighted. Different diagnostic tools that are currently used in Nepal for diagnosis of TB and drug susceptibility was also reiterated in the presentation. He then gave an overview of the TB control program in Nepal and its current status. The webinar also highlighted about drug resistance TB, causes, types and interventions for prevention. Finally, Dr. Yadav talked about National Strategic Plan strategies and how teamwork can help end TB as per the set targets.
The completion of the presentation was followed by ice-breaking Zoom polls focusing on understanding of the topic and about the Nepalese Society of Community Medicine (NESCOM). Some interesting questions were raised after the poll questions which the speaker answered with very much clarity and precision. The webinar lasted for 1 and half hours with 75 participants. The webinar ends with the concluding words by Dr. Rajiv Mani Adhikari (MC for the program) with the announcement of an upcoming webinar on “Sexual and reproductive health: adolescent friendly services center and its laws, implementation and challenges in Nepal” on 17th May, 2022.
Objectives of Webinar:
- To understand the global and regional burden of TB in Nepal.
- To understand the current scenario of TB in Nepal.
- To update on the latest diagnosis and treatment of TB.
- To update knowledge regarding MDR-TB, patient support and strategy for TB elimination in Nepal.
Key points that came out during the discussion:
- TB is an ancient disease present since mid 1800s. It was historically known as Wasting disease and White plague
- TB was declared as a global emergency by WHO in 1993. Though it is said to be a disease of poverty affecting mostly young adults, worldwide people are suffering from this disease. Majority of TB deaths occurs in the developing world with more than half of deaths due to TB occurring in Asia
- Worldwide, it is one of the top 10 causes of death with 1.3 million deaths among HIV negative and an additional 3,00,000 deaths among HIV positive. Globally, 10 million develop TB disease with 90% affected being adults (aged more than 15 years) and 9% affected being HIV positive
- End TB strategy was introduced in 2015 with vision of ending TB in Nepal by 2050. Ending TB is defined as a decrease in incidence rate of more than 80% by 2030 and 90% by 2035 compared to 2015 baseline
- TB burden in Nepal is quite alarming with around 1,17,000 people with TB currently living in Nepal with majority of them in Madhesh Pradesh (23%), Bagmati Pradesh (23%) and Lumbini Pradesh (21%)
- Though many cases are being detected each year, still around 41,500 cases are missed annually. The diagnostic tools used for diagnosis of TB are microbiological tests- smear microscopy, Cartridge Based Nucleic Acid Amplification Test (CBNAAT), culture and supportive tests- chest Xray, Tuberculin skin test (TST), Interferon Gamma Release Assays (IGRA), cytology: Fine needle aspiration cytology (FNAC), histopathology: biopsy
- TB burden is much higher, almost 1.6 times higher than previously estimated. Due to efforts on TB epidemiology in Nepal, there has been an estimated annual reduction of TB incidence by 3% in the last decade which is better than the global annual decline rate of 1.5%-2% but needs to be accelerated to meet the End TB targets
- National TB control program in Nepal started in 1994 with Directly Observed Treatment Short-course (DOTS) strategy which was quite effective followed by the Stop TB strategy introduced in 2006 which was a total failure. This ultimately has effect on achieving the targets and indicators of End TB strategy introduced in 2016
- Nepal falls under the 2nd highest burden country for MDR-TB. Drug resistance is confirmed if growth of M. Tuberculosis is observed in cultures despite presence of adequate concentration of first line anti TB drugs. Though Drug resistance tuberculosis (DR-TB) can be due to microbial, clinical, or programmatic, it essentially is a man-made phenomenon
- Inappropriate treatment from healthcare providers, inadequate supply and poor quality of drugs or inadequate drug intake or poor treatment response of the patient all may lead to DR-TB. DR-TB can further be divided in different types which includes Mono-resistance, Rifampicin resistance, Poly-resistance, Multi drug resistance, pre-extensive drug resistance and Extensive drug resistance
- Five principle ways of intervention can be adopted to prevent DR-TB:
- Early detection and high-quality treatment of drug-susceptible TB
- Early detection and high-quality treatment of drug-resistant TB
- Effective implementation of infection control measures
- Strengthening and regulation of health system
- Addressing underlying risk factors and social determinants
- To eliminate TB by 2025, National strategic plan has been put forward with strategies focused on Active case finding, TB co-morbidities, Private sector engagement, Drug resistant TB, Information Communication Technology (ICT) tools for adherence and monitoring, Preventive measures, Community engagement and Multisectoral response.
Point for the policy brief:
To End TB focus should be on Integrated, patient-centered TB care and prevention prioritizing research and innovation. Government of Nepal should implement bold policies and supportive system with strong Supervision, Monitoring and Evaluation to achieve the WHO End TB strategy
Points to be discussed in the executive committee:
1.Role of Nepalese Society of Community Medicine (NESCOM) for capacity building of Community Medicine residents and graduates for intensified research and innovation focused on Tuberculosis with experts in the field
2.Building partnership and cooperation with the National Tuberculosis Control Centre, Ministry of Health and Population, Government of Nepal in implementing TB control program
Conclusion:
Tuberculosis is still responsible for huge burden of communicable disease worldwide, in Southeast Asia and Nepal. If not intervened at this point of time, it will have huge impact in regard to mortality and morbidity of people with huge economical loss. Hence, it is necessary that the Government and Private health sector acts together with proper intersectoral coordination to eliminate this disease
